Post operative drains can be a blessing or a curse. Are they really needed for an abdominoplasty?
Abdominoplasty, commonly known as a tummy tuck, is a transformative procedure aimed at creating a firmer and more contoured abdominal profile by removing excess skin and fat and tightening the underlying muscles. While the surgical technique has advanced significantly over the years, one topic continues to generate debate: the necessity of post-operative drains. These small tubes, designed to remove excess fluid from the surgical site, have long been considered standard practice. But are they indispensable, or have modern advancements rendered them obsolete?
Watch a Abdominoplasty Procedure
If would like a visual video to see a actual abdominoplasty video, we have provided one in the link below of Dr. John Diaz performing a routine Abdominoplasty (Tummy Tuck) procedure. This will aid the following information in this article.
Disclaimer: Youtube Age Verfication Needed
Notice
Focus on the anatomy of the procedure, and how every step ties together precisely.
Key Ideas
What's the purpose of the procedure? How is it accomplished? What would you say is the most important step?
Understanding Post-Operative Drains
Post-operative drains are small silicone or plastic tubes placed during surgery to prevent the buildup of seromas—fluid collections that can form in the space between the skin and the abdominal wall. These tubes are connected to a bulb or collection device, allowing for the manual removal of accumulated fluid during the recovery period. Drains serve a crucial function by minimizing fluid retention, reducing swelling, and decreasing the risk of infection associated with stagnant fluid.
Understanding Post-Operative Drains
Post-operative drains are small silicone or plastic tubes placed during surgery to prevent the buildup of seromas—fluid collections that can form in the space between the skin and the abdominal wall. These tubes are connected to a bulb or collection device, allowing for the manual removal of accumulated fluid during the recovery period. Drains serve a crucial function by minimizing fluid retention, reducing swelling, and decreasing the risk of infection associated with stagnant fluid.
The Case for Drains in Abdominoplasty
The use of drains in abdominoplasty has been a cornerstone of post-operative care for decades. For complex procedures, such as those involving significant liposuction or extensive tissue removal, the placement of drains provides surgeons with a reliable method to manage fluid dynamics. By reducing the likelihood of seromas, drains contribute to a more predictable healing process and help avoid complications that could necessitate additional surgical intervention.
Moreover, the ability to monitor the volume and appearance of the fluid collected in the drain bulbs offers both patients and surgeons valuable insights into the recovery process. For instance, an unexpected increase in fluid output or a sudden change in its color may signal an issue that requires immediate medical attention.
Challenges and Limitations of Post-Op Drains
Despite their utility, drains are not without their challenges. Patients often find them cumbersome, particularly during the initial weeks of recovery. The tubes can cause irritation at the insertion site, and the task of emptying and cleaning the drainage bulbs may feel overwhelming for some. Additionally, the presence of drains creates an entry point for bacteria, increasing the risk of localized infections if proper hygiene protocols are not strictly followed.
Some patients also experience a psychological burden from the presence of drains, as they can serve as a visible reminder of their post-surgical vulnerability. For these reasons, alternatives to traditional drains have gained traction among both surgeons and patients in recent years.
The fluid removed by drains often includes a mix of blood and other serous fluids that naturally accumulate as part of the body’s inflammatory response to surgery. By providing an exit route for these fluids, drains play an important role in promoting smooth healing. However, they are not without drawbacks. Patients often report discomfort associated with their presence, and there is a risk of infection at the insertion site if proper care is not taken.
Pros
Have been standard practice for a long time to help reduce swelling post op and have proven track record.
Cons
Discomfort can be a issue, potential risk of infection if not properly taken care of drain sites, and mental/visual aspect of drain.
Exploring Drain-Free Techniques
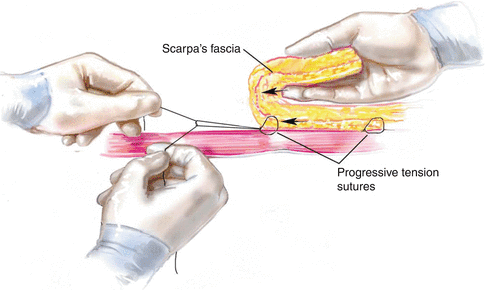
Advancements in surgical methods have led to the development of drain-free abdominoplasty techniques, such as the use of progressive tension sutures (PTS). These sutures are strategically placed to eliminate dead space between the skin and underlying tissues, thereby reducing the potential for fluid accumulation. By anchoring the skin more securely to the abdominal wall, PTS not only minimizes the need for drains but also provides additional support for the healing process.
Studies comparing traditional and drain-free techniques have shown promising results. In many cases, the rate of seroma formation with progressive tension sutures is comparable to or even lower than that observed with traditional drain usage. Furthermore, patients who undergo drain-free procedures often report greater comfort and an overall smoother recovery experience.
However, it is important to note that not all patients are ideal candidates for drain-free methods. Factors such as the extent of the surgery, the patient’s body mass index (BMI), and their overall health profile can influence the choice of technique. For example, individuals undergoing extensive body contouring or those with pre-existing conditions that affect wound healing may still benefit from the added security provided by traditional drains.
Progressive Tension Sutures (PTS) Graphic
Eliminates Dead Space
This helps reduce the posibility of seroma formation and infection.
Allows To Be Drain Free Post Op
More comfort for the patient and eliminates possibility of drain sites getting infected.
More Comfort and Support For Abdomen
Adds a extra layer of support to the abdomen by securing it more and post op care will be more comfortable for the patient.
Balancing Patient Comfort and Clinical Outcomes
The decision to use drains or adopt a drain-free approach ultimately lies in the hands of the surgeon, guided by the unique needs and preferences of the patient. For surgeons, the challenge is to strike a balance between ensuring optimal clinical outcomes and prioritizing patient comfort. This decision-making process often involves a thorough assessment of the surgical plan, as well as a detailed discussion with the patient about their recovery expectations.
Conclusion
The necessity of post-operative drains in abdominoplasty remains a nuanced topic with valid arguments on both sides. While traditional drains offer a tried-and-true method for managing fluid accumulation and reducing complications, innovations such as progressive tension sutures provide viable alternatives for many patients. Ultimately, the choice between these approaches depends on the surgeon’s expertise, the complexity of the procedure, and the patient’s individual circumstances.